Known as "beta blockers" - Introduction
Dr Angelo Pieris. Teaching Fellow in Clinical Pharmacology and Therapeutics. Barts & The London Medical School.
Updated by Dr Hew Torrance, July 2013.
The sympathetic nervous system affects all organs in order for the body to maintain optimal organ perfusion and prioritise certain sensory and motor functions in various circumstances. This is classically termed the fight or flight enabling response.
Here is a starter..
What is the effect on cardiac muscle and bronchial wall smooth muscle of sympathetic stimulation?
Known as "beta blockers" - Pharmacology

When will there be increased sympathetic nervous system stimulation of the heart?
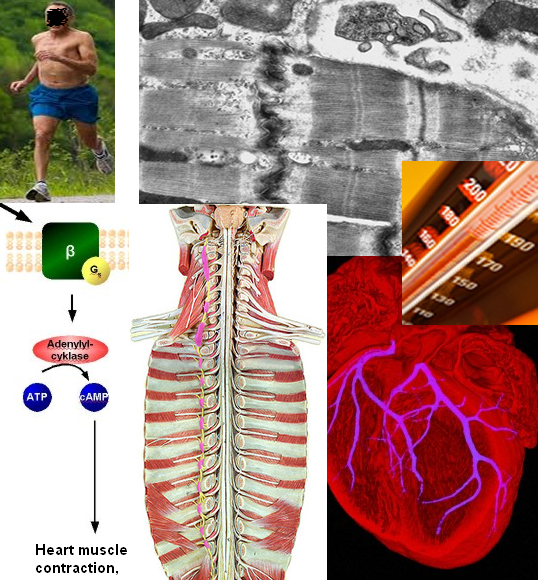
Sympathetic nervous stimulation of the heart increases heart rate and contractility. This happens after the release of neurotransmitters noradrenaline and adrenalin. These act on the mainly beta 1 type of adrenergic nerve receptors in the heart, including those of the sino-atrial (SA) node, the primary pacemaker.
Adrenaline from the adrenal glands is secreted into the bloodstream and thus has a systemic effect. Noradrenaline is released from the nerve terminals and has a local effect.
Why are we dealing with terms like "beta 1" not just "adrenoceptor" antagonists?
The adrenoceptors vary a little. This variability has been targeted by pharmacologists. For example the lungs display more beta 2 receptors than the heart which has more beta 1 receptors. This has led to the development of medicines that are designed to work on specific receptors (adrenoceptors). The idea is to avoid unwanted adverse effects. Salbutamol for example is a beta 2 agonist. But it still affects the heart and causes a tachycardia. In reality there is overlap with "selective" adrenergic medication.
So avoid beta blockers in people with asthma and those little blue inhalers?
Yes.
Why might the above scenario cause a problem if the man had ischaemic heart disease?
If there is narrowing of the coronary arteries due to atherosclerosis then myocardial metabolism increases above the level at which oxygen and nutrient supply can be increased to the myocytes.
If the beta adrenoceptors are blocked by a drug how will this help the patient to avoid angina pain? (Imagine a patient who is walking, not running!)
The autonomic stimulus caused by exertion is reduced. There is a less increase in myocardial oxygen and nutrient demand as the heart rate and contractility does not rise as it would otherwise have done. The other aspect to this is that a "beta blocked" person may not be able to act as vigorously as before. This can be socially and physically limiting.
Pharmacology
A sixty year old woman who normally takes metoprolol 50mg twice daily undergoes drainage of a peri-anal abscess under general anaesthetic. She has been nil-by mouth for eighteen hours as her operation kept being pushed back due to other emergencies taking priority. Unfortunately she goes into fast AF in recovery. The anaesthetist decides to give her a dose of metoprolol by intravenous injection.
Based on the information above (And the BNF) what intravenous dose might be given of the same beta-blocker?
Known as "beta blockers" - Indications
In which of the conditions mentioned below are beta blockers recognized as a treatment option?
Cardiovascular indications for the use of beta blockers:
Other uses:
Contra-indications:
Hypertension
Are ACE-Inhibitors and calcium channel blockers not used to treat hypertension instead of beta blockers?
All these drugs are used to treat high blood pressure. The evidence suggests that white and Asian people under 55 are often benefit from ACE-Inhibitors most, whilst black and over 55 year olds are often given calcium channel blockers first.
Why the ethnic divide?
Black people often have low-renin hypertension, so gain less benefit from ACE-inhibitors.
Heart Failure
Why use beta blockers in heart failure? Should these people not be on infusions of noradrenaline instead??
Beta blockers are strongly indicated in stable heart failure and are associated with decreased mortality. For the reasons stated on the previous page. Another reason for this is that patients with heart failure are at high risk of death from developing sudden cardiac arrhythmias. Beta blockers reduce the incidence of such arrhythmias.
The key principle to bear in mind is that they are NOT given to patients in a de-compensated state, i.e. patients who have suddenly developed symptoms such as pulmonary oedema, who may have difficulty maintaining a satisfactory blood pressure for adequate organ perfusion.
So how should they be used in treating heart failure?
They are started at a very low dose, the patient may initially feel worse. Functional benefit may not be apparent for weeks. The drugs slow the progression of disease and reduce deaths from arrythmias.
Atrial fibrillation.
Is that when the atria go wobbly?
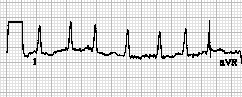
Well the AV node is no longer the pacemaker, there is disorganised contraction. The atria dilate.
It can be new onset or recurrrent, symptomatic or asymptomatic, caused by a variety of disease or idiopathic.
So what use are beta blockers?
They are useful if the patient is symptomatic. They can slow the ventricular rate. In patients that have paroxysmal AF they can keep the patient in sinus rythmn.
In the treatment of atrial fibrillation which is most accurate?
A patient on the acute medical unit is diagnosed with an acute coronary syndrome. The consultant sees him on admission and decides to start a beta blocker.
What evidence is that based on?
A 15% reduction in mortality in the first week following myocardial infarction (MI) was reported by the ISIS1 study.
When is a beta blocker contra-indicated in MI patients?
Known as "beta blockers" - Adverse Effects
Potentially dangerous adverse effects :
Case. The next three questions fit together.
Mr Bashir is a 72 year old who was admitted with chest pain 24 hours ago. He has a past medical history of angina. His medications are aspirin, bisoprolol, simvastatin, and isosorbide mononitrate.
You are the F1 on call. You are asked to review him because the nurse has found his blood pressure to be 109/60 and his pulse to be 55.
What do you do first?
Mr Bashir is sitting in a chair drinking a cup of tea, smiles and greets you as he sees you approaching.
You ask him how he is doing.
What might issues you specifically want to explore with the patient in this short consultation?
Mr Bashir tells you that he is looking forward to being able to go home now that he is feeling pain free and is able to gently move around without any symptoms. He is willing to endure percutaneous angioplasty if he is advised to do so.
You discuss your findings with the nurse and agree a plan which is:
Rita Ryvita is a well sixty four year old with essential hypertension. She has no hypertension related organ damage. Her GP starts bisoprolol 2.5mg once daily and follows the patient up a month later. On her return visit the patient reports no adverse symptoms. The GP checks her blood pressure, which is found to be 149/85 and then increases the bisoprolol to 5 mg.
What follow up blood tests for drug monitoring the does Rita require?